Anxiety
What is anxiety?
Causes, Symptoms, Types, Tips for Recovery, Social Anxiety, Panic Attacks Treatment Options and Natural Alternatives for Anxiety
Depression
What is anxiety?
Causes, Symptoms, Types, Tips for Recovery, Treatment Options and Natural Alternatives for Anxiety
Stress
What is anxiety?
Causes, Symptoms, Types, Tips for Recovery, Treatment Options and Natural Alternatives for Anxiety
ADD / ADHD
What is anxiety?
Causes, Symptoms, Types, Tips for Recovery, Treatment Options and Natural Alternatives for Anxiety
Sleep Difficulty
What is anxiety?
Causes, Symptoms, Types, Tips for Recovery, Treatment Options and Natural Alternatives for Anxiety
Kids & Teens
What is anxiety?
Causes, Symptoms, Types, Tips for Recovery, Treatment Options and Natural Alternatives for Anxiety
- Rebel With a Cause: Why It’s Right to Speak up When the Crowd Is Wrong
- Deadly Brain-Eating Amoeba Strikes Again: What You Need to Know
- Shades of Gray or Black-And-White: Why the Color of Your Thinking Matters
- Put Down the Pasta: That New Study About Noodles Is Nonsense
- Better Late Than Never: Finally, the Truth About Butter Is Revealed
- Prohibition, Politics, and Profit: The Truth About Cannabis and Why Government Wants to Control It
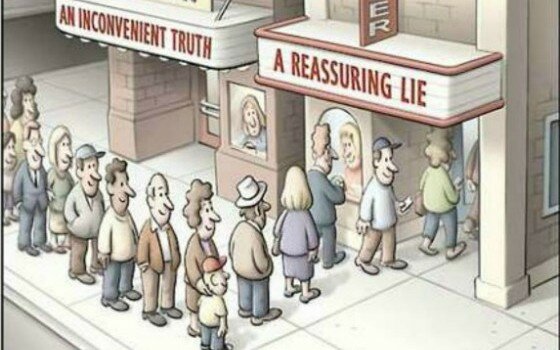
- You Can’t Handle the Truth: How Confirmation Bias Distorts Your Opinions
- Pass the Butter, Skip the Sugar: We’ve Been Told Big Fat Lies About Heart Disease
- Diabetes: What You Need to Know About This Killer Disease
- A Tale of Grapes, Politics, Cults, and Aliens: Why People Cling to False Beliefs
- Just Following Orders: It Is Shockingly Easy to Get People to Do Bad Things
- Creative High School Students Invent Better Light Therapy Device for SAD Sufferers
- Deadly Brain-Eating Amoeba Strikes Again: What You Need to Know
- Put Down the Pasta: That New Study About Noodles Is Nonsense
- Better Late Than Never: Finally, the Truth About Butter Is Revealed
- Benefits Without the Buzz: Juicing Cannabis for Health
- Artificial Sweetener Use During Pregnancy Linked to Overweight Babies
- Big Pharma’s Big Lies: Why Painkiller Addiction Is at Epidemic Levels in the US
- 1 in 3 Antibiotics Prescribed in US Are Unnecessary, Study Finds
- This Is Now the Third Leading Cause of Death in the United States
- New Rx? Take One Chocolate Bar and Call Me in the Morning
- Carrots, Not Sticks: Junk Food Junkies Go Healthy When Rewarded
- Your Lifestyle Impacts Your Gut Bacteria – and Ultimately, Your Overall Health
- Study Links Common Medications to Brain Shrinkage and Dementia
- Would You Like a Side of Phthalates With That Burger?
- Pass the Butter, Skip the Sugar: We’ve Been Told Big Fat Lies About Heart Disease
- Which Is More Stressful: Uncertainty or Inevitable Pain?
- Who Is More Negative – Conservatives or Liberals?
- The Strange Link Between Parasites, Cats, and Explosive Rage
- Adults Fail Miserably at This, and It Is Killing Us
- Sunbathing Is Linked to Longer Life, Study Says
- Why You Should Trust Your “Aha!” Moments
- Yikes! 60% of Our Diet Is Made up of This, and It Is Scary Stuff
- Scrap the Scale, Banish BMI: This Number Is Far More Important
- Warning: Adderall Can Cause Schizophrenia-Like Psychosis
- Love Chocolate? Sweet News – It Might Make You Smarter!

- Rebel With a Cause: Why It’s Right to Speak up When the Crowd Is Wrong
- Shades of Gray or Black-And-White: Why the Color of Your Thinking Matters
- How to Talk to Your Children About Tragic Events
- Big Pharma’s Big Lies: Why Painkiller Addiction Is at Epidemic Levels in the US
- You Can’t Handle the Truth: How Confirmation Bias Distorts Your Opinions
- Is Caring About What Others Think Holding You Back?
- Small Changes or Life Overhaul? The Answer May Surprise You
- Why You Should Trust Your “Aha!” Moments
- Scrap the Scale, Banish BMI: This Number Is Far More Important
- How to Quit Smoking: Know Yourself
- How to Quit Smoking: Know Your Enemy
- A Tale of Grapes, Politics, Cults, and Aliens: Why People Cling to False Beliefs
- How to Quit Smoking: Are Irrational Beliefs Getting in Your Way?
- Just Following Orders: It Is Shockingly Easy to Get People to Do Bad Things
- What’s the Best Way to Overcome Your Fears? Face Them.
- Why Making Certain Foods Forbidden Makes You Crave Them More
- Are You Your Own Worst Enemy?
- 15 Productivity Hacks That Will Make Your Life Easier
- Feeling Like a Fraud? How to Overcome Impostor Syndrome
- Will You Read This Article?
- This Time Will Be Different: How to Finally Succeed at Your New Year’s Resolutions
- Everything You Need to Know About ADHD
- Stop It! These Habits Are Bad for Your Mental Health
- Everything You Need to Know About Anxiety in Children
- When Thinking Becomes Harmful: Rumination, Depression, and Anxiety
- See All Insight Answers…
- Click To Ask Jake A Question…